 Bioidentical Hormones Found Beneficial After Hysterectomy
Bioidentical Hormones Found Beneficial After Hysterectomy
by Jeffrey Dach MD
Should My Ovaries Be Removed ?
Forty Three year old Eva sought medical advice about irregular bleeding from massive uterine fibroids. The continuous bleeding interfered with her lifestyle and caused severe fatigue from the iron deficiency anemia.
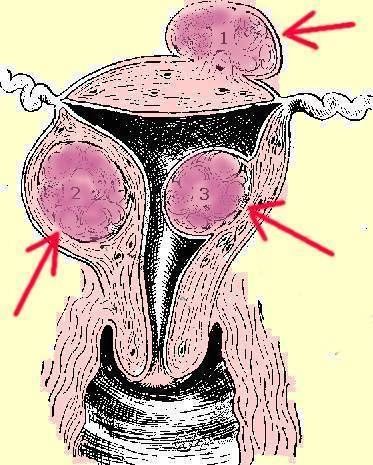
I had previously proposed uterine artery embolization, but the consulting interventional radiologist instead recommended hysterectomy because the fibroids were too large for his procedure. Eva went home, and after thinking for a few days, finally accepted she would have to undergo surgery. Left image: Diagram of cross section of uterus. Red Arrows point to uterine fibroids . Courtesy of wikimedia commons.
What are Uterine Fibroids?
Uterine fibroids are benign growths in the uterus that can grow to large size causing irregular bleeding and pressure on the abdominal organs. They are fairly common and can be detected with pelvic examination, and confirmed with pelvic sonogram and MRI scan. Massive uterine fibroids are most commonly treated with surgery, a hysterectomy operation which removes the uterus and fibroid tumors. Treatment is usually successful with a good outcome.
Visiting the OB Gyne Surgeon
Next, Eva paid a visit to the OB GYNE surgeon to discuss her operation. The surgeon recommended a COMPLETE hysterectomy with removal of both ovaries. Sitting in the surgeon's office, Eva timidly protested. "Why remove my ovaries?" asked Eva. The surgeon replied, "Removing the ovaries eliminates the chance of ovarian cancer, and you don't need them anyway."
 To Remove or Not to Remove the Ovaries? That is the Question
To Remove or Not to Remove the Ovaries? That is the Question
So now Eva was again in my office asking for my opinion. Should she go against the surgeon's advice and insist on preserving her ovaries, or should she follow the surgeon's advice to have a COMPLETE hysterectomy with removal of the ovaries ?
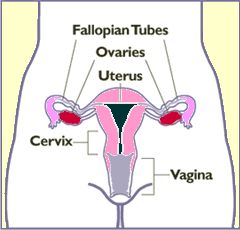
Left Image : Diagram showing Ovaries (in red). Uterus is Pink. Courtesy of Wikimedia Commons.
The ovaries are important because they are the hormone factories that pump out women's hormones on a daily basis. Removing the ovaries removes the source of women's hormones causing all hormone levels to decline to low levels, immediately sending the woman into Menopause.
Left image: Surgeons performing hysterectomy courtesy of wikimedia commons.
Studies Show Removing Ovaries Increases Mortality
 Luckily, the answer to Eva's question can be found in the medical literature. William Parker MD and Cathleen Rivera MD reported that removing the ovaries is detrimental to overall health and results in increased mortality. (1)(2)
Luckily, the answer to Eva's question can be found in the medical literature. William Parker MD and Cathleen Rivera MD reported that removing the ovaries is detrimental to overall health and results in increased mortality. (1)(2)
Dr. Parker followed 30,000 women for 24 years after their hysterectomy. Half had ovaries removed and half had ovaries preserved. The group with ovaries removed did, in fact, have a lower rate of ovarian and breast cancer. However, this was overshadowed by a marked increase in death from heart disease and other cancers. The group with the ovaries removed had a higher all cause mortality rate, and therefore Dr. Parker recommended that women preserve the ovaries in the pre-Menopausal age group. Dr Parker also found that postoperative hormone replacement is very beneficial at reducing heart disease risk. (1)
In a second study, Dr Cathleen Rivera followed 1,000 Pre-Menopausal women (under age 45) after hysterectomy, and found that removal of the ovaries resulted in a disturbing 84% increase in death from heart disease. However, if these women were given estrogen replacement after ovarian removal, they were protected with a 35% decrease in mortality from heart disease.(2) I thought this was rather impressive.
Bioidentical Hormones After Hysterectomy
 These two studies provide convincing evidence of the health benefits of hormone replacement after hysterectomy. Although the patients in these two studies were given Premarin which is a natural hormone (from a pregnant horse), we find that a cocktail of bioidentical hormones including estradiol, estriol, progesterone, DHEA and testosterone works as well or better than the horse hormones. Since all women are humans, we I consider it preferable to prescibe human hormones rather than hormones from pregnant horse urine (Premarin).
These two studies provide convincing evidence of the health benefits of hormone replacement after hysterectomy. Although the patients in these two studies were given Premarin which is a natural hormone (from a pregnant horse), we find that a cocktail of bioidentical hormones including estradiol, estriol, progesterone, DHEA and testosterone works as well or better than the horse hormones. Since all women are humans, we I consider it preferable to prescibe human hormones rather than hormones from pregnant horse urine (Premarin).
Left Image: pregnant horse, courtesy of wikimedia commons. Why use horse hormones when human hormones are available?
What about preventing ovarian cancer and breast cancer in high risk groups?
For women at high risk with familial breast and ovarian cancer, and positive BRCA genetic markers, Dr Parker says it makes sense to go ahead with removing the ovaries for these people in high risk groups.
Articles with Related Interest:
The Importance of BioIdentical Hormones by Jeffrey Dach MD
The Safety Of Bio-Identical Hormones by Jeffrey Dach MD
Breast Cancer Prevention and Iodine Supplementation by Jeffrey Dach MD
Jeffrey Dach MD
7450 Griffin Rd Suite 180/190
Davie, FL 33314
Phone: 954-792-4663
Facebook
Blog
Links and References
(1) http://www.ncbi.nlm.nih.gov/pubmed/19384117
http://www.hgos.org/resources/OBGYN_Article.pdf
http://www.doctorsinfoweb.com/pdf/NHS_green_J_William_Parker-p1027.pdf
http://www.hopeforfibroids.org/pdf/NHS_green_J_William_Parker-p1027.pdf
Obstet Gynecol. 2009 May;113(5):1027-37.
Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses' health study. Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, Shoupe D, Berek JS, Hankinson S, Manson JE. John Wayne Cancer Institute at Saint John's Health Center, Santa Monica, California 90401, USA. Comment in:
OBJECTIVE: To report long-term health outcomes and mortality after oophorectomy or ovarian conservation.
METHODS: We conducted a prospective, observational study of 29,380 women participants of the Nurses' Health Study who had a hysterectomy for benign disease; 16,345 (55.6%) had hysterectomy with bilateral oophorectomy, and 13,035 (44.4%) had hysterectomy with ovarian conservation. We evaluated incident events or death due to coronary heart disease (CHD), stroke, breast cancer, ovarian cancer, lung cancer, colorectal cancer, total cancers, hip fracture, pulmonary embolus, and death from all causes.
RESULTS: Over 24 years of follow-up, for women with hysterectomy and bilateral oophorectomy compared with ovarian conservation, the multivariable hazard ratios (HRs) were 1.12 (95% confidence interval [CI] 1.03-1.21) for total mortality, 1.17 (95% CI 1.02-1.35) for fatal plus nonfatal CHD, and 1.14 (95% CI 0.98-1.33) for stroke. Although the risks of breast (HR 0.75, 95% CI 0.68-0.84), ovarian (HR 0.04, 95% CI 0.01-0.09, number needed to treat=220), and total cancers (HR 0.90, 95% CI 0.84-0.96) decreased after oophorectomy, lung cancer incidence (HR=1.26, 95% CI 1.02-1.56, number needed to harm=190), and total cancer mortality (HR=1.17, 95% CI 1.04-1.32) increased.
For those never having used estrogen therapy, bilateral oophorectomy before age 50 years was associated with an increased risk of all-cause mortality, CHD, and stroke. With an approximate 35-year life span after surgery, one additional death would be expected for every nine oophorectomies performed.
CONCLUSION: Compared with ovarian conservation, bilateral oophorectomy at the time of hysterectomy for benign disease is associated with a decreased risk of breast and ovarian cancer but an increased risk of all-cause mortality, fatal and nonfatal coronary heart disease, and lung cancer. In no analysis or age group was oophorectomy associated with increased survival.
(2) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2755630/?tool=pubmed
Menopause. 2009 Jan–Feb; 16(1): 15–23.
Increased cardiovascular mortality following early bilateral oophorectomy
Cathleen M. Rivera, MD,1 Brandon R. Grossardt, MS,2 Deborah J. Rhodes, MD,1 Robert D. Brown, Jr., MD, MPH,3 Véronique L. Roger, MD, MPH,4,5 L. Joseph Melton, III, MD, MPH,5 and Walter A. Rocca, MD, MPH3,5
We conducted a cohort study with long-term follow-up of women in Olmsted County, MN, who underwent either unilateral or bilateral oophorectomy before the onset of menopause from 1950 through 1987. Each member of the oophorectomy cohort was matched by age to a referent woman from the same population who had not undergone any oophorectomy. We studied the mortality associated with cardiovascular disease in a total of 1,274 women with unilateral oophorectomy, 1,091 women with bilateral oophorectomy, and 2,383 referent women.
Results: Women who underwent bilateral oophorectomy before age 45 years experienced an increased mortality associated with cardiovascular disease compared with referent women (HR, 1.44; 95% CI, 1.01–2.05; P = 0.04).
Within this age stratum, the HR for mortality was significantly elevated in women who were not treated with estrogen through age 45 years or longer (HR, 1.84; 95% CI, 1.27–2.68; P = 0.001) but not in women treated (HR, 0.65; 95% CI, 0.30–1.41; P = 0.28; test of interaction, P = 0.01). Mortality was further increased after excluding deaths associated with cerebrovascular causes.
Conclusions: Bilateral oophorectomy performed before age 45 years is associated with increased cardiovascular mortality, especially with cardiac mortality. However, estrogen treatment may reduce this risk.
From a clinical perspective, our findings suggest that women who underwent bilateral oophorectomy at a young age are at increased risk of cardiovascular death, especially of cardiac death. This increased mortality may be attenuated by adequate estrogen treatment. Our findings provide new evidence to guide the individualized assessment of the risks and benefits of prophylactic bilateral oophorectomy in young women.1,4–6,8,14 This preventive practice currently involves approximately 4.5 million women older than 55 years living in the United States who have undergone bilateral oophorectomy before reaching natural menopause.28,34
In addition, our findings provide observational evidence for a long-term cardiovascular protective effect of estrogen either naturally produced by the ovaries or given as treatment to women who underwent bilateral oophorectomy at younger ages. These findings emphasize the importance of estrogen treatment after the surgery.6,9–14
We focused our analyses on age at estrogen deficiency rather than on the length of estrogen treatment after the surgery to study the combined effects of age at the surgery and length of treatment.
Several studies have shown increased cardiovascular mortality in women who experienced early menopause (before age 45 years) from either natural or medical causes,35–40 and a statistical model has linked prophylactic bilateral oophorectomy before age 65 years with an increase in overall mortality and coronary heart disease mortality.1,4,5
Similarly, in the Women’s Health Initiative Observational Study, hysterectomy plus oophorectomy performed over a broad age range was a significant predictor of cardiovascular disease during a short-term follow-up.28
Recent analyses from the Women’s Health Initiative Coronary Artery Calcium Study showed an increased risk of subclinical coronary artery disease in women who underwent both hysterectomy and bilateral oophorectomy and were not treated with estrogen compared to women who underwent hysterectomy alone. The increased risk was independent of traditional cardiovascular risk factors.12
Our results for estrogen treatment after bilateral oophorectomy are consistent both with findings from previous clinical studies40–44 and with findings from animal studies. Primates who underwent premenopausal oophorectomy and did not receive exogenous estrogen had significantly accelerated atherosclerosis compared with those that did not have oophorectomy
This study showed that women who underwent early bilateral oophorectomy are at increased risk of death involving cardiovascular disease, especially cardiac diseases. However, treatment with estrogen through age 45 years or longer may reduce this risk. These findings, in conjunction with the results of other studies,1,4,5,8 have important clinical implications and should prompt a reassessment of prophylactic bilateral oophorectomy in premenopausal women.6,14
http://www.businesswire.com/portal/site/home/permalink/?ndmViewId=news_view&newsId=20090420005411&newsLang=en
April 20, 2009 New Study Finds Removing Ovaries During Hysterectomy Increases Risk of Death, Outweighs Benefits
SANTA MONICA, Calif.--(BUSINESS WIRE)--Results of a landmark study led by a doctor at John Wayne Cancer Institute at Saint John’s Health Center raises serious questions about the long-term survival benefits of removing a woman’s ovaries during routine hysterectomy. The study, appearing in the May 2009 issue of Obstetrics and Gynecology, compared women with benign (noncancerous) reproductive disease who were given a hysterectomy, with either bilateral oophorectomy (removing both ovaries) or ovarian conservation (leaving the ovaries intact).
http://www.news-medical.net/news/2009/04/20/48588.aspx
Removal of ovaries during hysterectomy increases risk of death, outweighs benefits 20. April 2009 23:32
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with
his/her personal physicians and to only act upon the advice of his/her
personal physician. Also note that concerning an answer which appears as
an electronically posted question, I am NOT creating a physician —
patient relationship.
Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved
This article may be reproduced on the internet without permission,
provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation